Estimated read time: 4 minutes
Every morning, Dr. Sarah Chen walks into her family practice knowing that alongside caring for patients, she’ll spend hours navigating the labyrinth of insurance paperwork. Like 92% of physicians surveyed by the American Medical Association, she agrees that prior authorization processes significantly influence her ability to practice medicine appropriately. If this sounds familiar, you’re not alone4and there are proven strategies to reclaim your time without compromising accuracy.
The 2025 healthcare landscape brings both challenges and opportunities. With new CMS reforms targeting electronic prior authorization implementation by 2026 and major health plans committing to streamline processes, now is the perfect time to optimize your administrative workflows.
92%
Physicians Affected
Report that prior authorization significantly impacts their practice
$23K
Annual Cost
Average practice spends per physician on authorization admin
50%
Time Reduction
Possible savings with electronic prior authorization systems
Understanding Prior Authorization: The Foundation of Efficient Paperwork
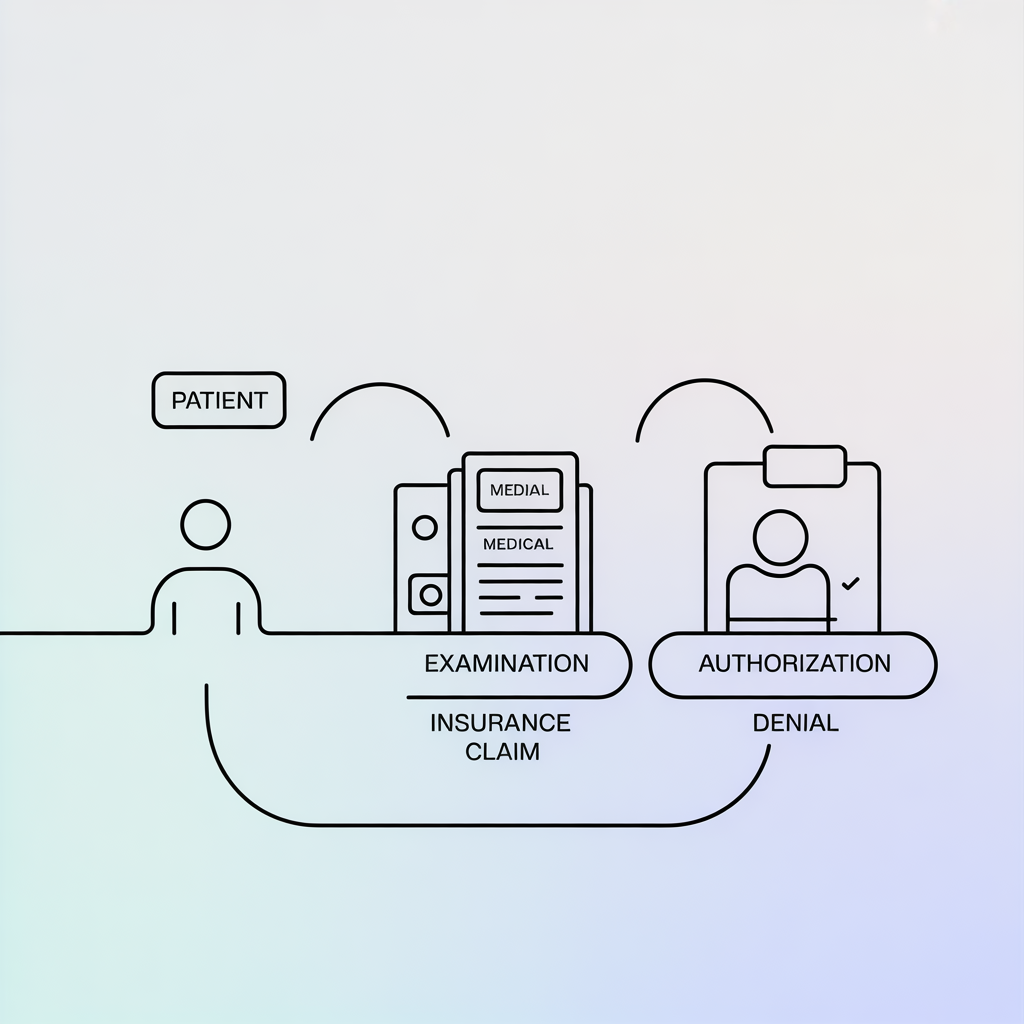
Prior authorization is the insurance requirement that physicians obtain approval before providing certain treatments, medications, or procedures. Think of it as a checkpoint system where insurers evaluate medical necessity before covering costs.
Here’s how it typically works: You submit a request detailing the patient’s condition, proposed treatment, and clinical justification. The insurer reviews this information against their coverage criteria and either approves, denies, or requests additional information.
Example: A patient with chronic back pain needs an MRI. Instead of ordering it immediately, you must first submit prior authorization showing that conservative treatments (physical therapy, medications) have been attempted and failed.
While designed to control costs and prevent unnecessary procedures, prior authorization has become a significant administrative burden. The good news? Strategic approaches can dramatically reduce the time and complexity involved.
Tip 1: Implement Electronic Prior Authorization Systems
The Problem
Manual, paper-based submissions are slow, error-prone, and time-consuming.
The Solution
Electronic prior authorization (ePA) systems can reduce
processing time by up to 50% and minimize errors.
Practical Implementation:
- Invest in practice management software with built-in ePA capabilities
- Train your staff on electronic submission workflows
- Use templates for common procedures to ensure consistency
- Integrate ePA systems with your Electronic Health Records (EHR)
Real-World Impact: Dr. Martinez’s orthopedic practice saw a 40% reduction in authorization processing time after implementing an integrated ePA system, freeing up three hours daily for patient care.
Tip 2: Create Standardized Documentation Templates
The Problem
Inconsistent documentation leads to denials and resubmissions.
The Solution
Develop comprehensive templates that include all necessary information insurers typically require.
Patient demographics and insurance information
ICD-10 diagnosis codes with specific clinical details
CPT procedure codes with medical necessity justification
Previous treatment history and outcomes
Supporting clinical documentation (labs, imaging reports)
Provider credentials and facility information
Pro Tip: Create specialty-specific templates. A cardiology practice needs different standard information than a dermatology office.
Tip 3: Establish a Dedicated Prior Authorization Workflow
The Problem
Ad hoc authorization handling creates delays and oversights
The Solution
Designate specific team members and create clear processes for handling different types of authorizations.
01
Identification Phase
Flag procedures requiring authorization during scheduling or visit planning
02
Preparation Phase
Gather all necessary documentation before submission
03
Submission Phase
Submit complete requests through appropriate channels
04
Follow-up Phase
Track submissions and respond promptly to requests for additional information
05
Communication Phase
Notify patients and providers of authorization status
Staff Assignment Example:
- Medical assistant identifies authorization needs during appointment scheduling
- Prior authorization specialist prepares and submits requests
- Practice manager handles denials and appeals
Tip 4: Build Strong Relationships with Insurance Representatives

The Problem
Generic, impersonal interactions with insurers slow down the process.
The Solution
Develop professional relationships with insurance representatives and understand each plan’s specific requirements.
Maintain Contact Lists
Keep a contact list of representatives for each major insurance plan
Attend Training Sessions
Participate in insurer-hosted webinars and training sessions
Join Advisory Committees
Participate in physician advisory committees when available
Document Requirements
Record each plan's preferred submission methods and requirements
Example: Dr. Johnson’s pediatric practice maintains a spreadsheet with contact information, preferred communication methods, and specific requirements for each insurance plan’s prior authorization department.
Tip 5: Leverage Technology and Data Analytics
The Problem
Lack of visibility into authorization patterns and approval rates.
The Solution
Use data analytics to identify trends and optimize your approach.
Key Metrics to Track:
- Approval rates by insurance plan and procedure type
- Average processing time for different types of requests
- Common denial reasons and patterns
- Cost of administrative time spent on authorizations
Technology Tools:
- Practice management dashboards that track authorization metrics
- Automated reminder systems for follow-ups
- Integration between EHR and authorization platforms
- Mobile apps for real-time status checking
Actionable Insights:
If data shows that Plan X denies 80% of MRI requests initially but approves 90% on appeal with additional documentation, you can proactively include that documentation in initial submissions.
The Business Case for Streamlined Processes
Consider the financial impact: The average physician practice spends $23,274 annually per physician on prior authorizationrelated administrative costs. Implementing these five strategies can reduce this burden by 30-50%, translating to significant cost savings and improved physician satisfaction.
Moreover, with upcoming regulatory changes4including the 2025 CMS commitment to standardize electronic submissions using FHIR-based APIs4practices that optimize now will be better positioned for future requirements
Moving Forward: Your Next Steps
Streamlining insurance paperwork isn’t just about efficiency4it’s about reclaiming time for what matters most: patient care. Start with one or two of these strategies and gradually build a comprehensive system that works for your practice.
The healthcare industry is evolving rapidly, with new tools and regulations emerging regularly. By implementing these evidence-based strategies, you’re not just solving today’s challenges4you’re building a foundation for future success.

What’s been your biggest challenge with insurance paperwork? Which of these strategies do you think would have the
most immediate impact in your practice? Share your experiences in the comments below, and let’s continue this
important conversation about reducing administrative burden while maintaining the highest standards of patient care.
References
- American Medical Association. (2024). AMA prior authorization physician survey. Retrieved from https://www.amaassn.org/practice-management/prior-authorization
- Centers for Medicare & Medicaid Services. (2025). CMS finalizes rule to expand access to health information and improve the prior authorization process. Retrieved from https://www.cms.gov/newsroom/press-releases/cmsfinalizes-rule-expand-access-health-information-and-improve-prior-authorization-process
- U.S. Department of Health and Human Services. (2025, June 23). HHS Secretary Kennedy, CMS Administrator Oz secure industry pledge to fix broken prior authorization system. Retrieved from https://www.hhs.gov/press-room/kennedy-ozcms-secure-healthcare-industry-pledge-to-fix-prior-authorization-system.html
- American College of Physicians. (2024). Toolkit: Addressing the administrative burden of prior authorization. Retrieved from https://www.acponline.org/advocacy/state-health-policy/toolkit-addressing-the-administrative-burden-of-priorauthorization
- National Center for Biotechnology Information. (2018). Streamlining the insurance prior authorization debacle. PMC6140260. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140260/
- CNBC. (2025, June 23). Prior authorizations: U.S. insurers to change approval process. Retrieved from https://www.cnbc.com/2025/06/23/prior-authorizations-us-insurers-to-change-approval-process.html
The administrative burden of prior authorization consumes valuable time that could be spent on patient care. By avoiding these common mistakes, you can navigate the system more efficiently while advocating for the systemic changes our patients deserve.