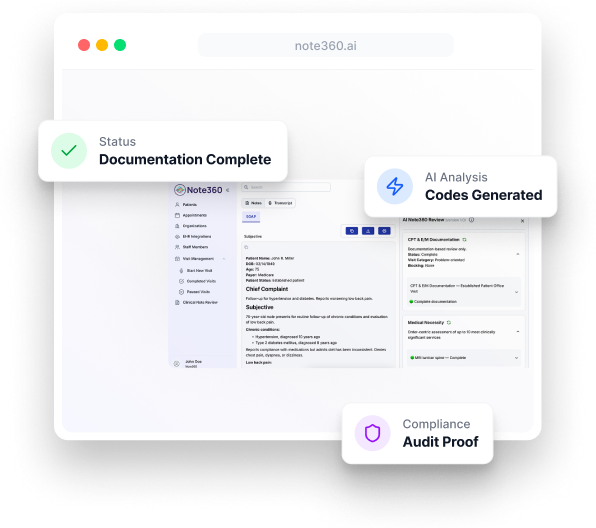
Welcome to a clearer way to document care. With Note360, clinicians can strengthen documentation clarity, support medical necessity, and reduce rework — right at the point of care.
See it in your workflow today.
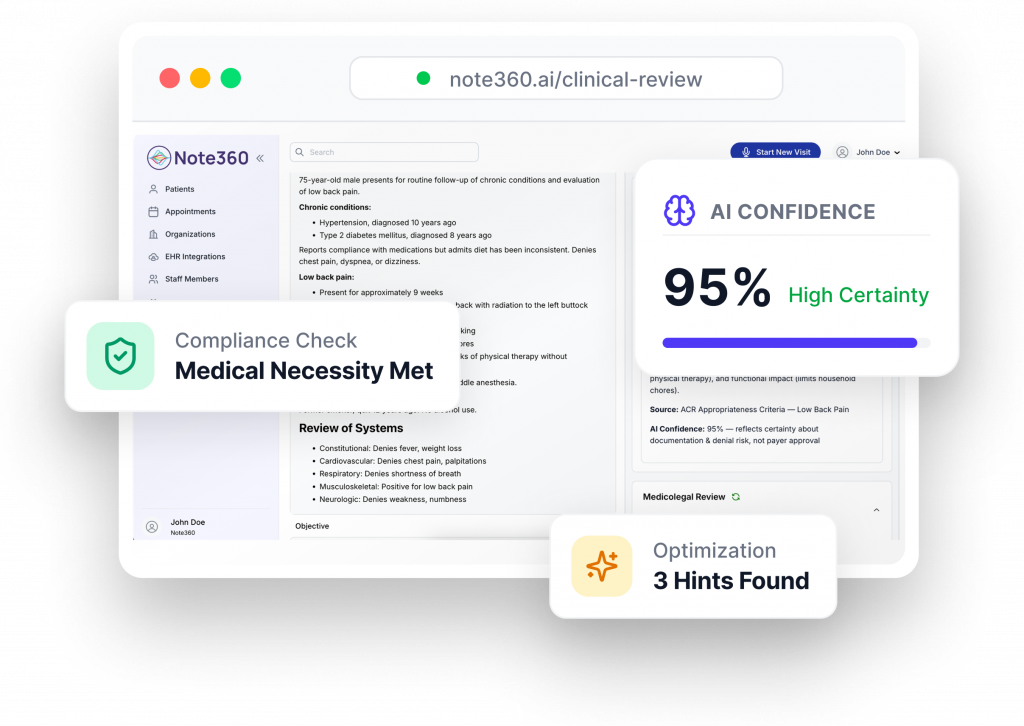
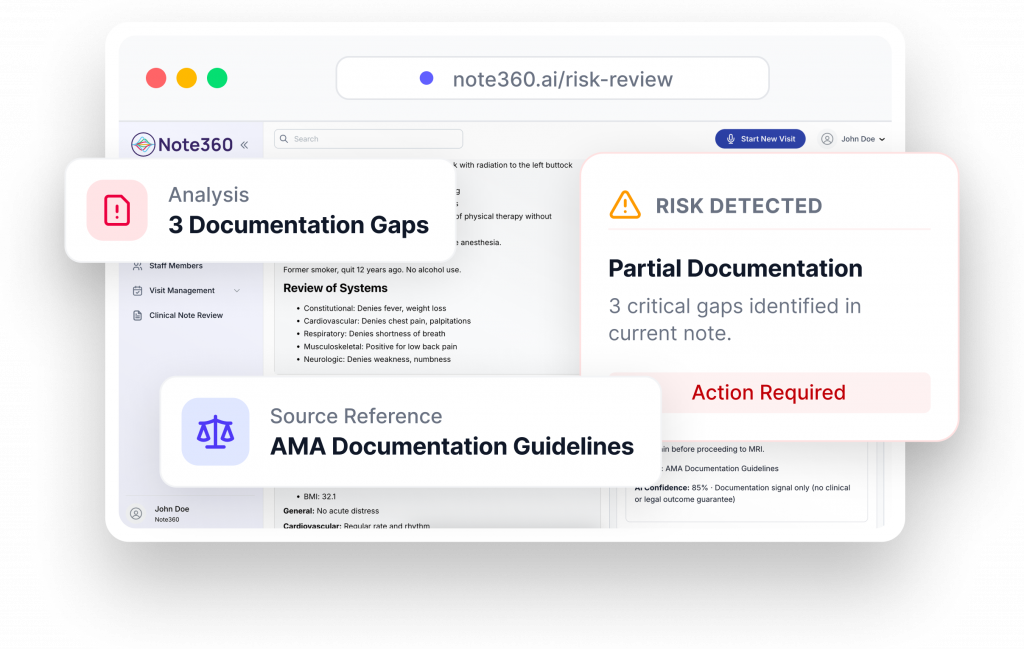
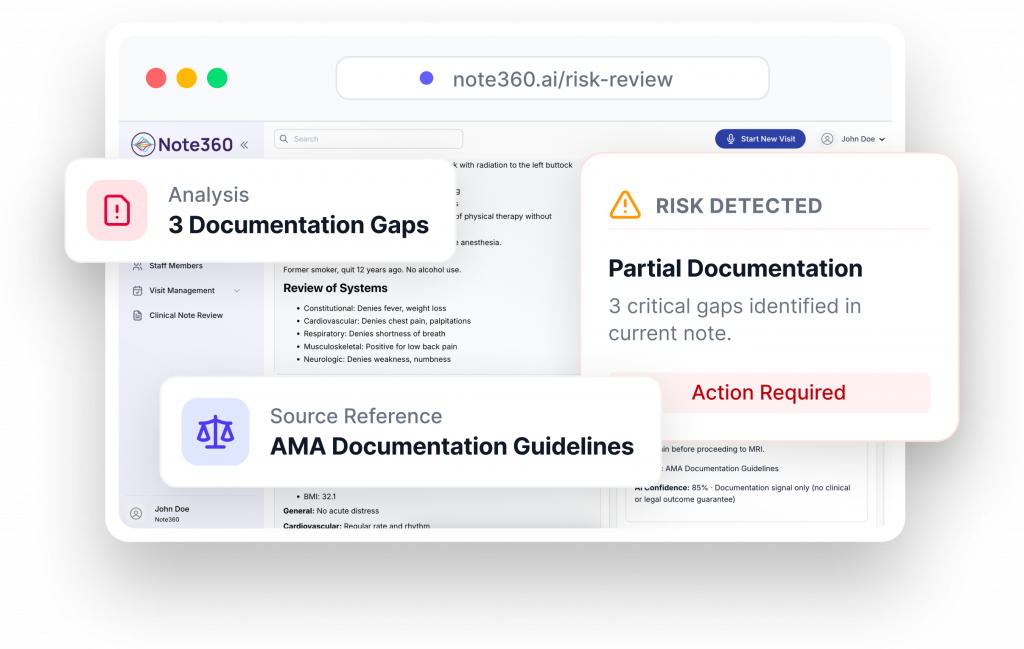
See documentation clarity while notes are being written.
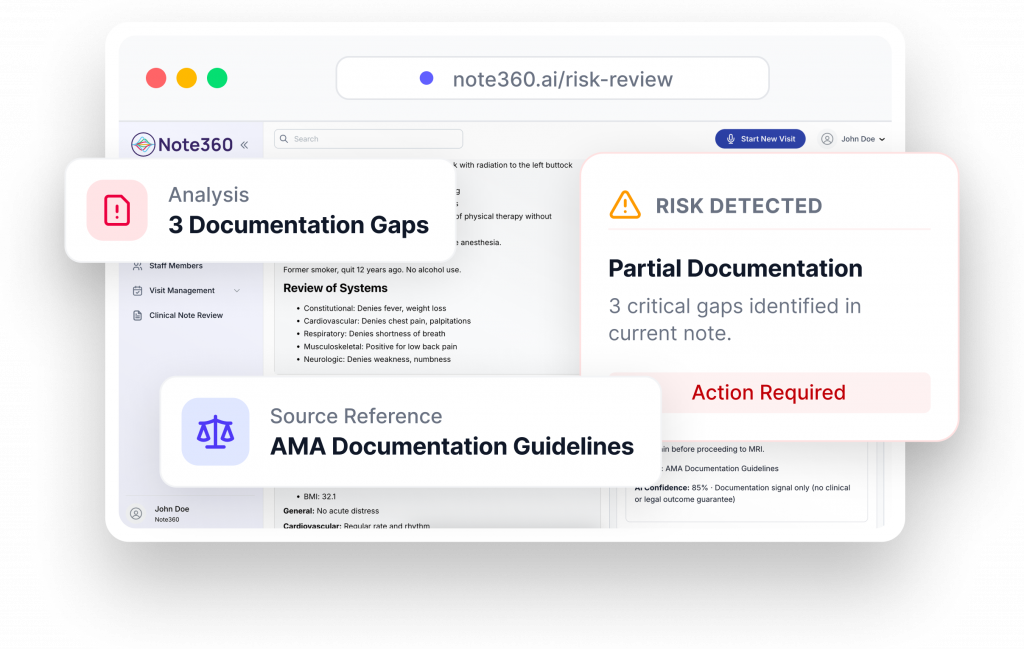
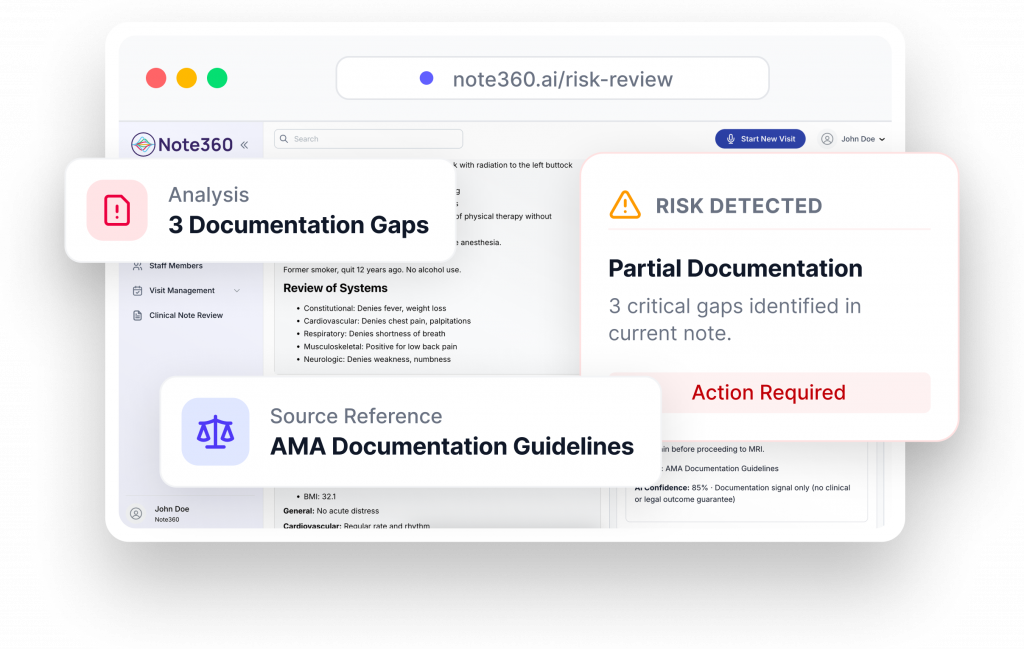
Note360 reviews only what is documented and highlights areas that may be unclear, incomplete, or missing important clinical context. By bringing visibility earlier in the workflow, clinicians and teams can address documentation gaps while the encounter is still fresh.
How it helps
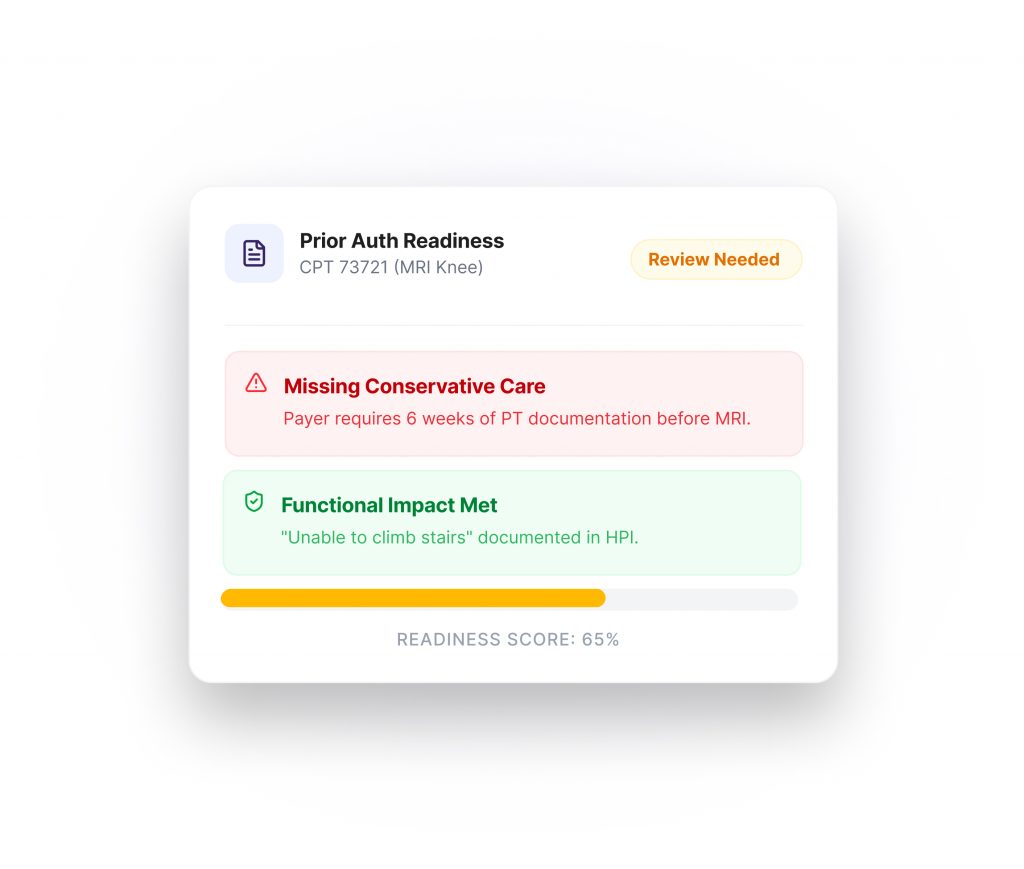
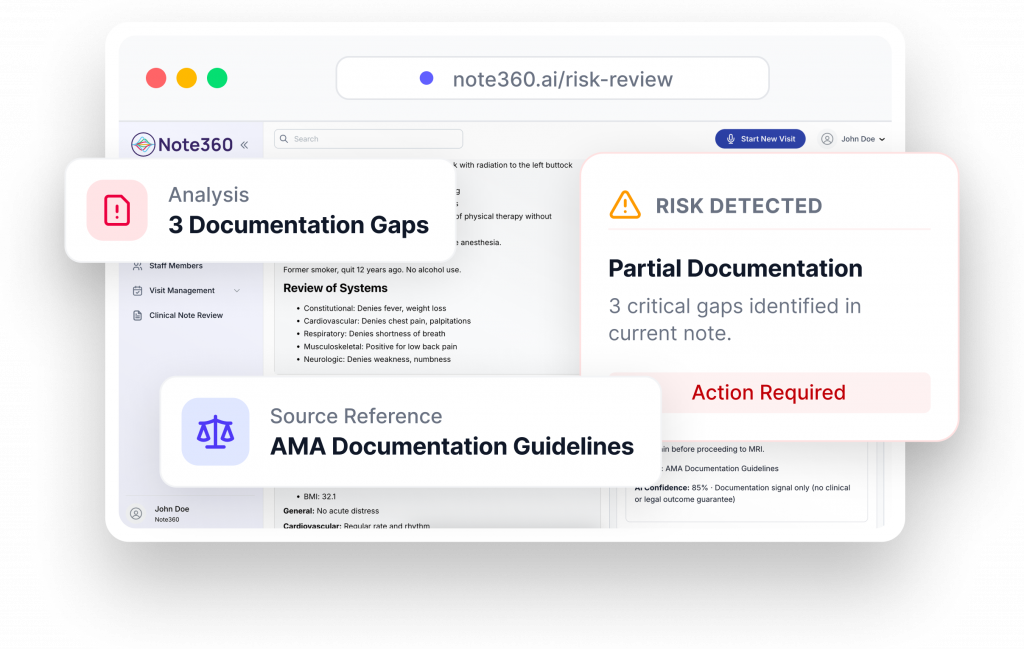
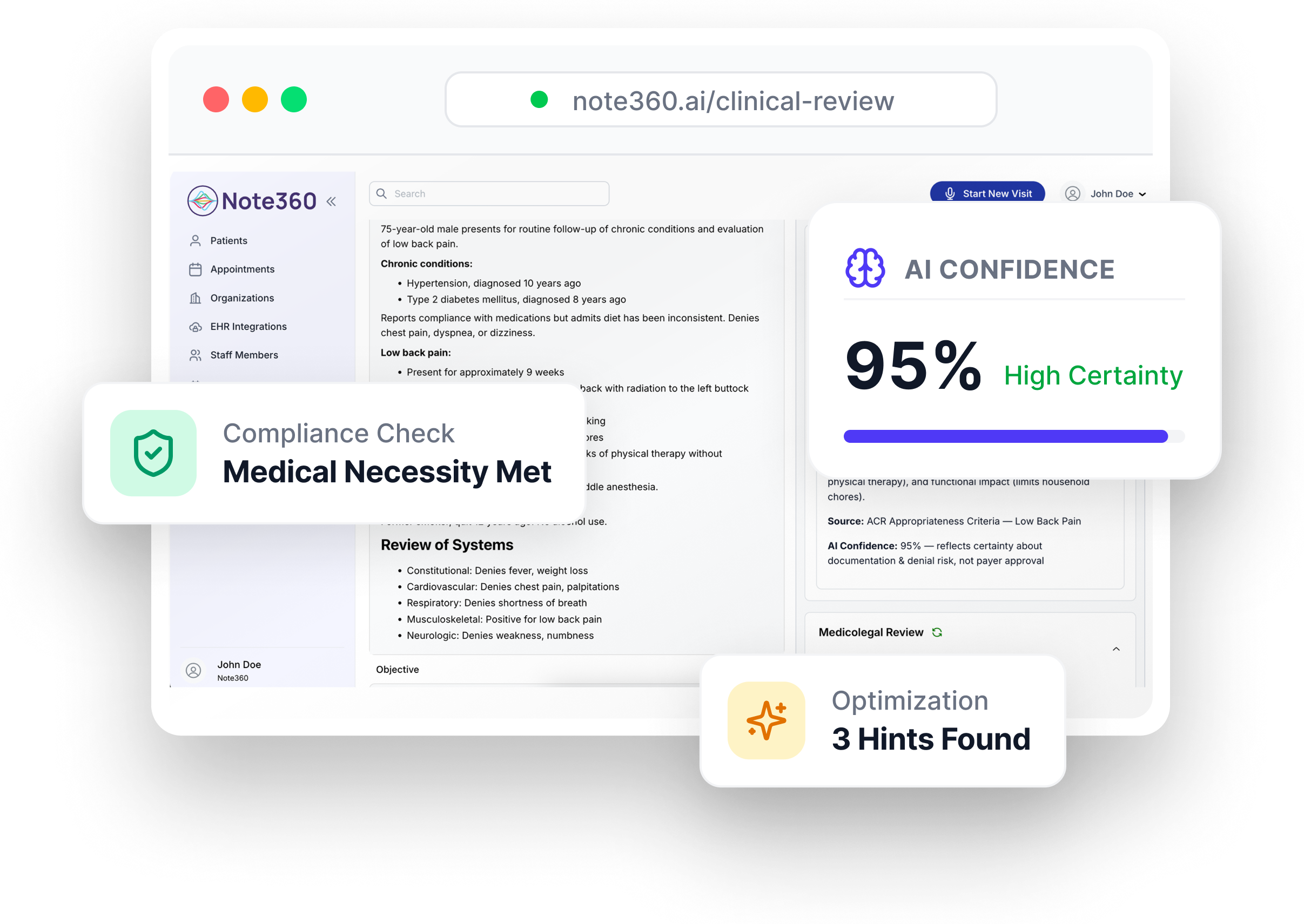
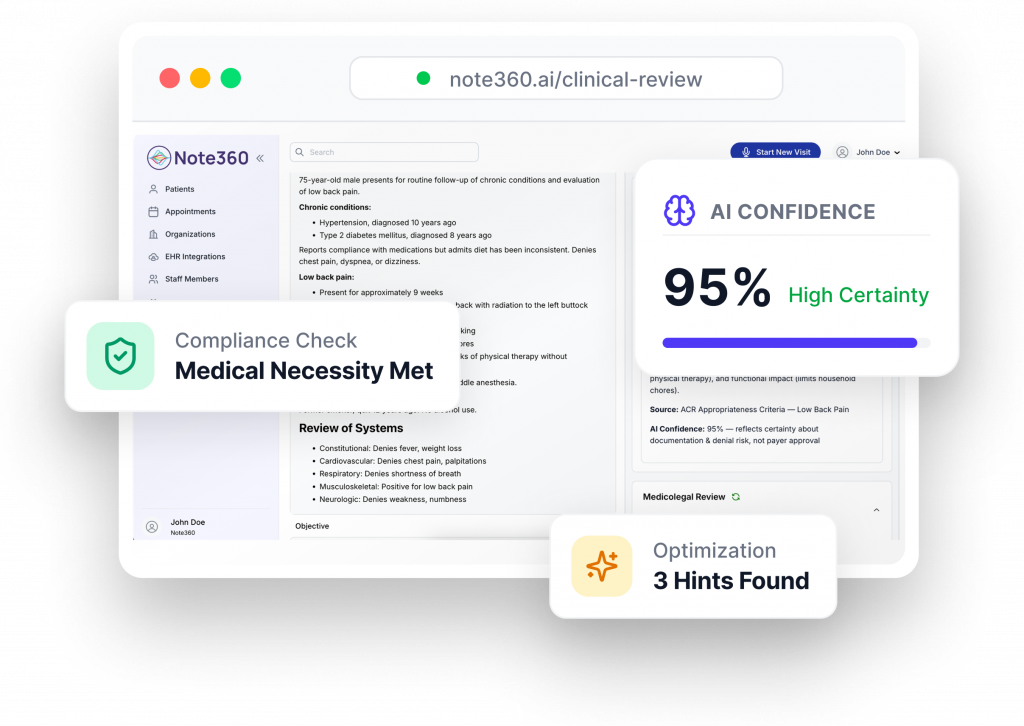
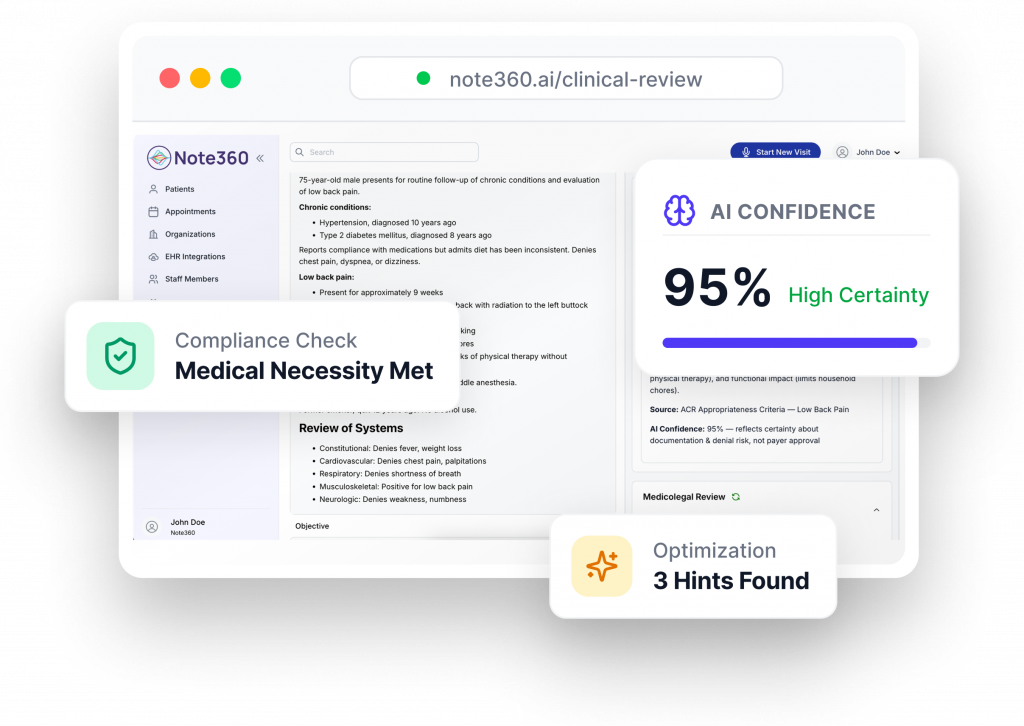
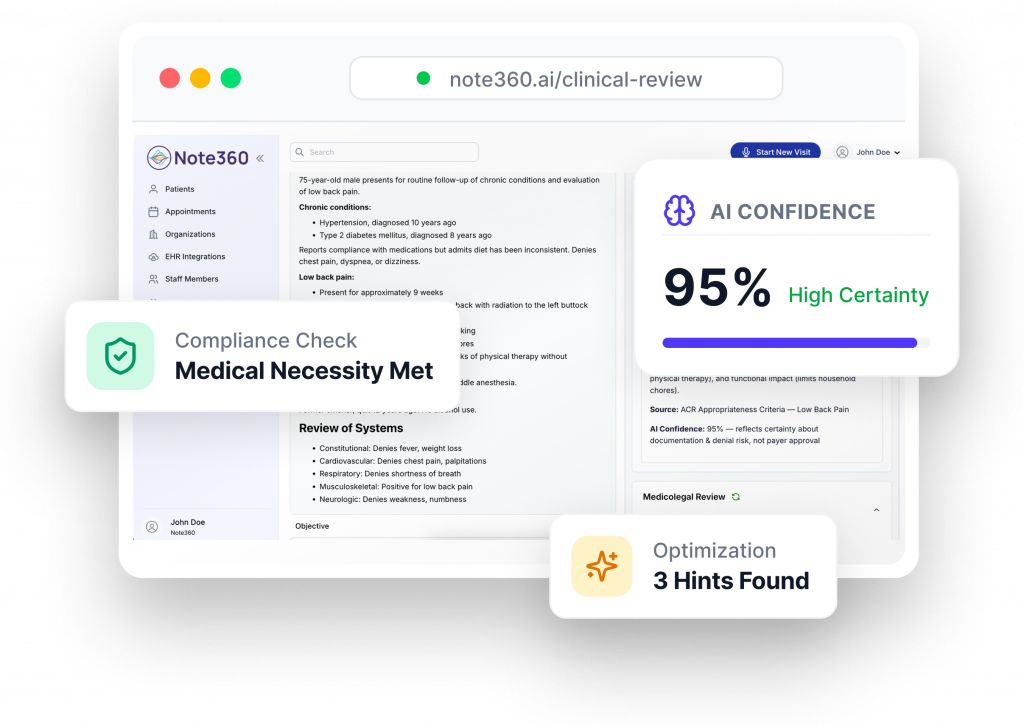
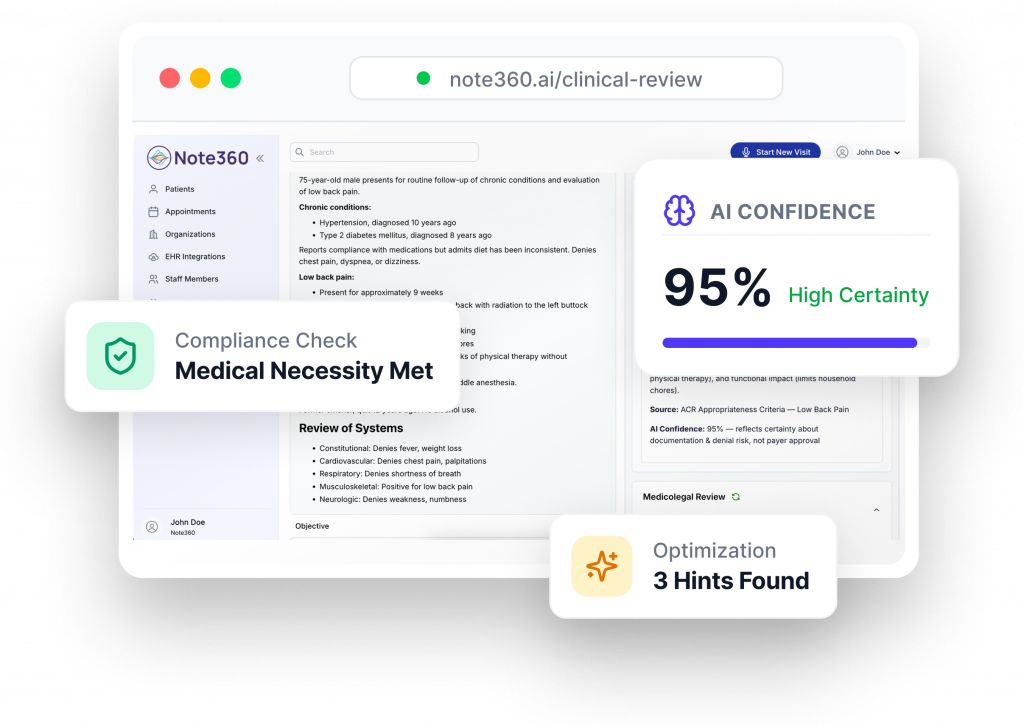
Understand whether documentation clearly supports medical necessity.
Note360 compares documented elements to guideline-based criteria and highlights where documentation may or may not clearly support medical necessity. Insights are educational, explainable, and source-cited.
How it helps
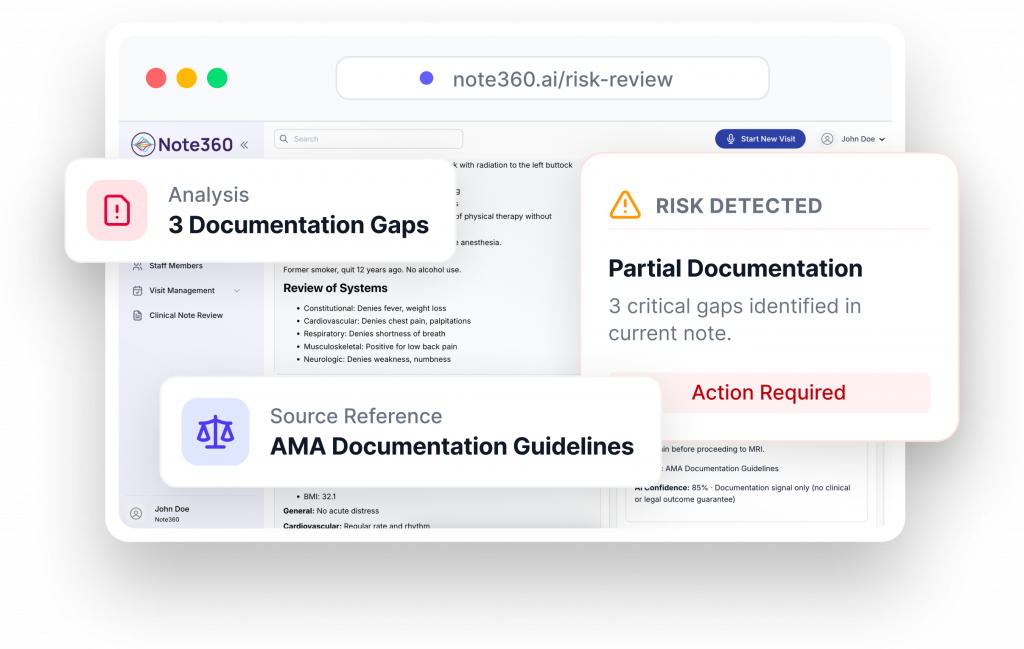
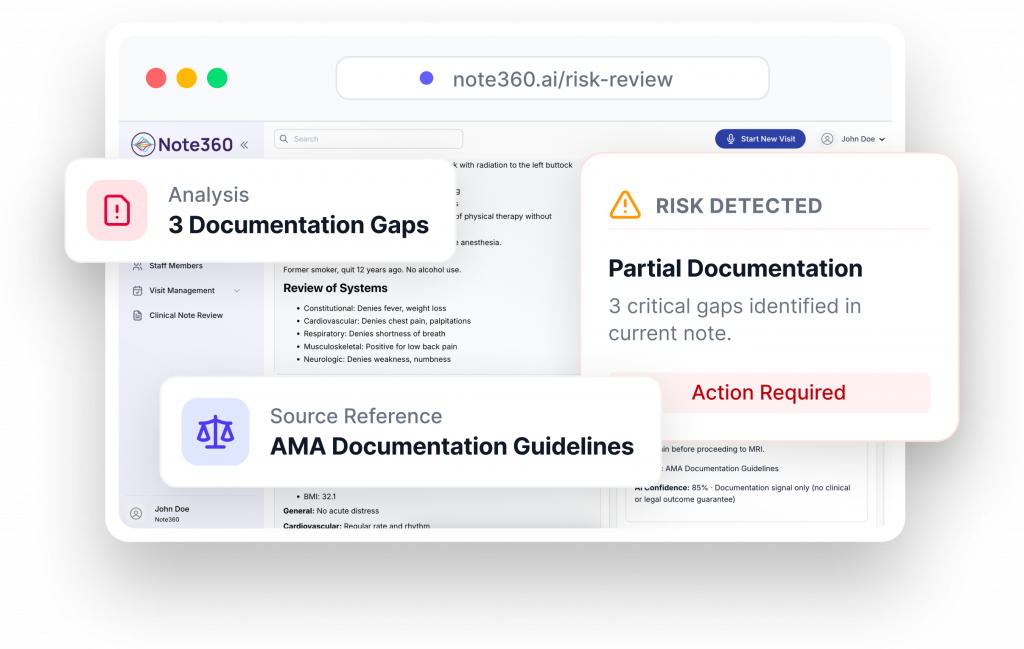
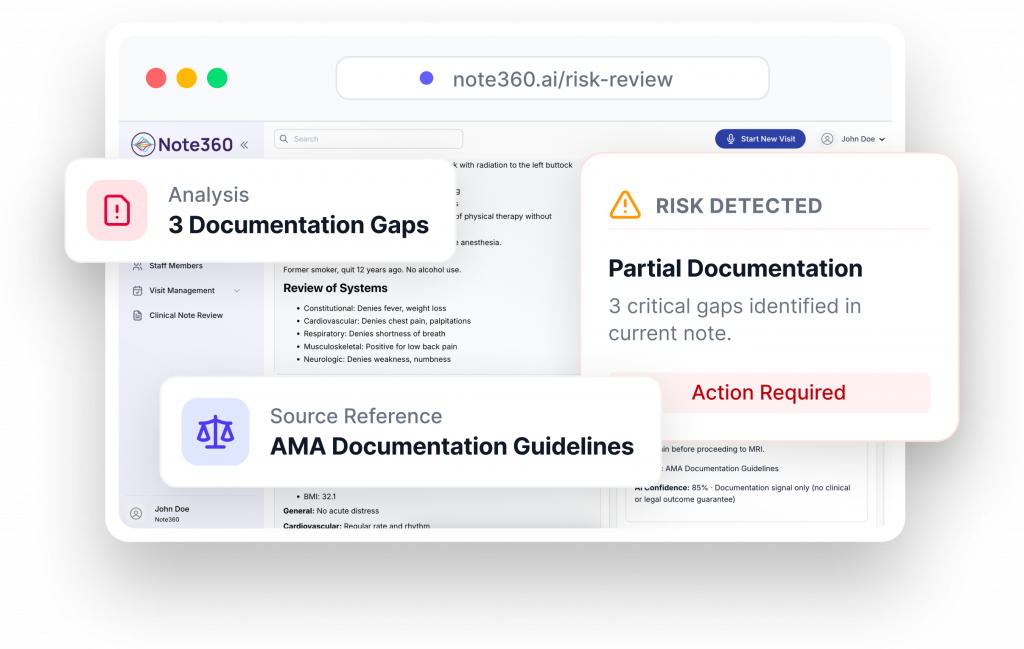
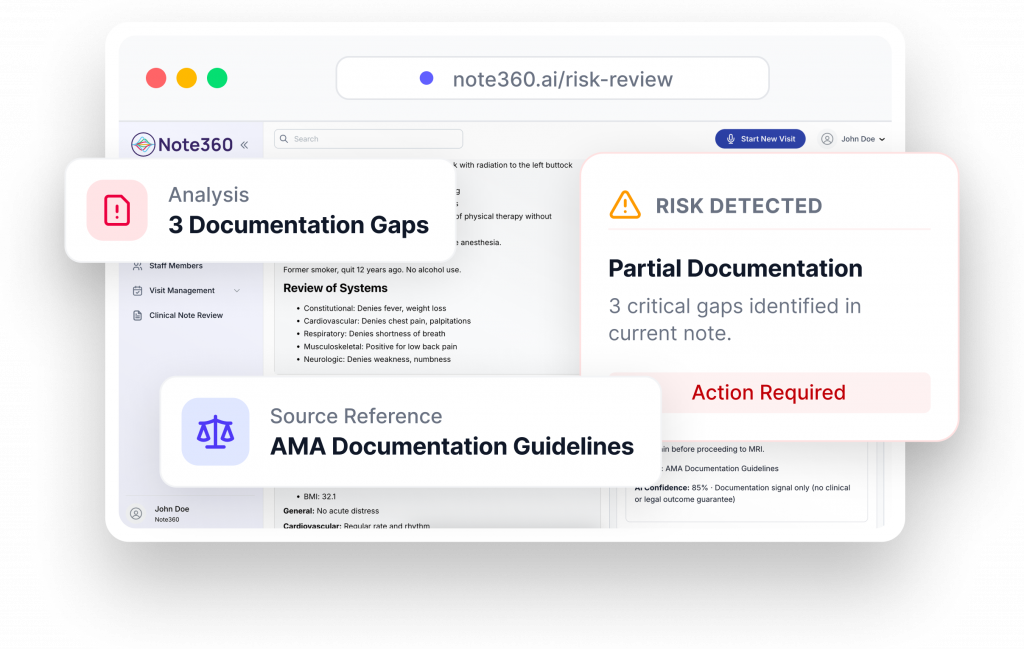
Extend documentation insight beyond the point of care.
In addition to real-time, point-of-care analysis, Note360 provides retrospective documentation review to help teams identify recurring documentation patterns and gaps that may affect compliance, reimbursement, and documentation integrity.
This review is designed to complement point-of-care intelligence, offering longitudinal insight rather than replacing real-time guidance.
How it helps
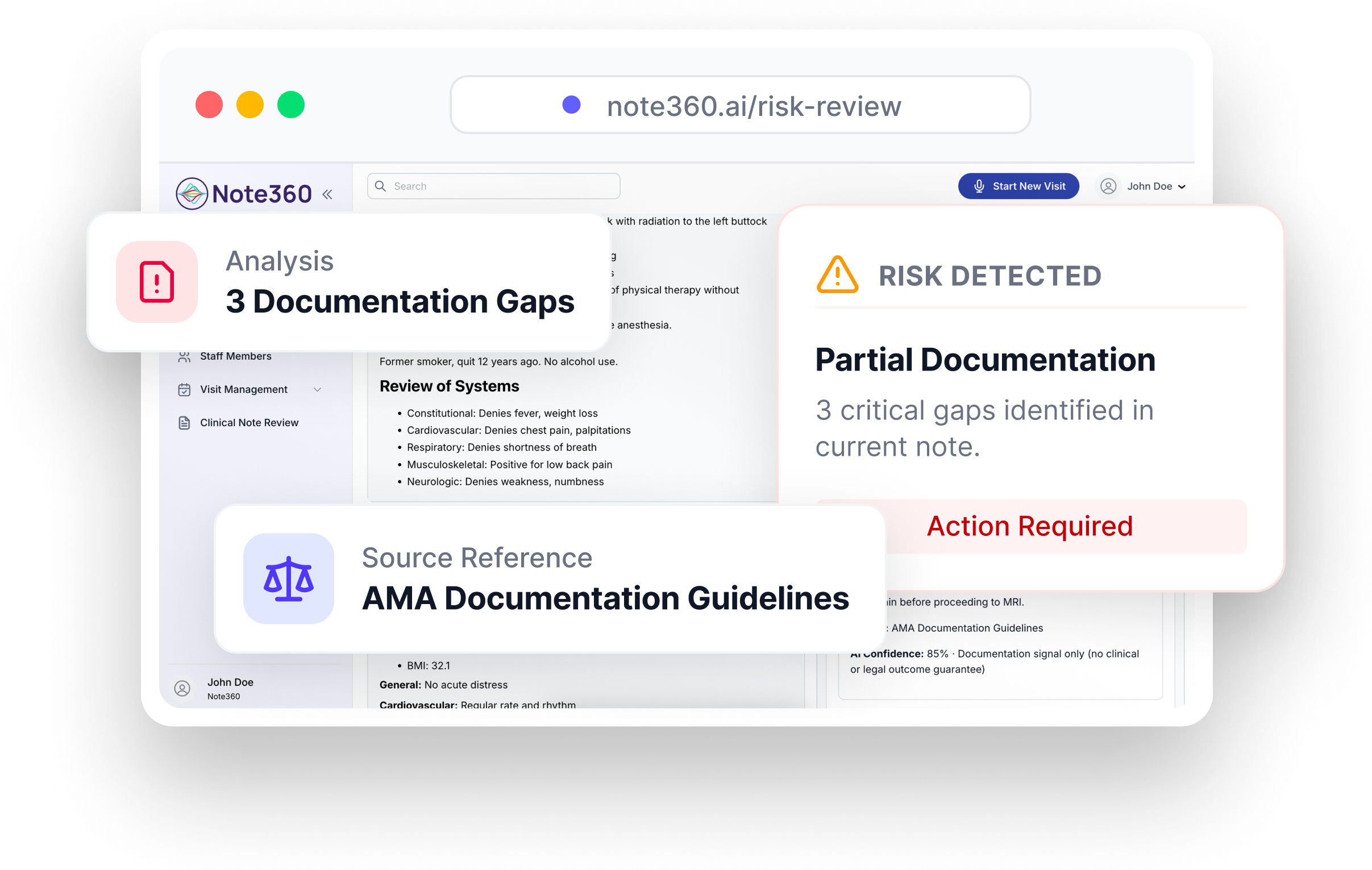
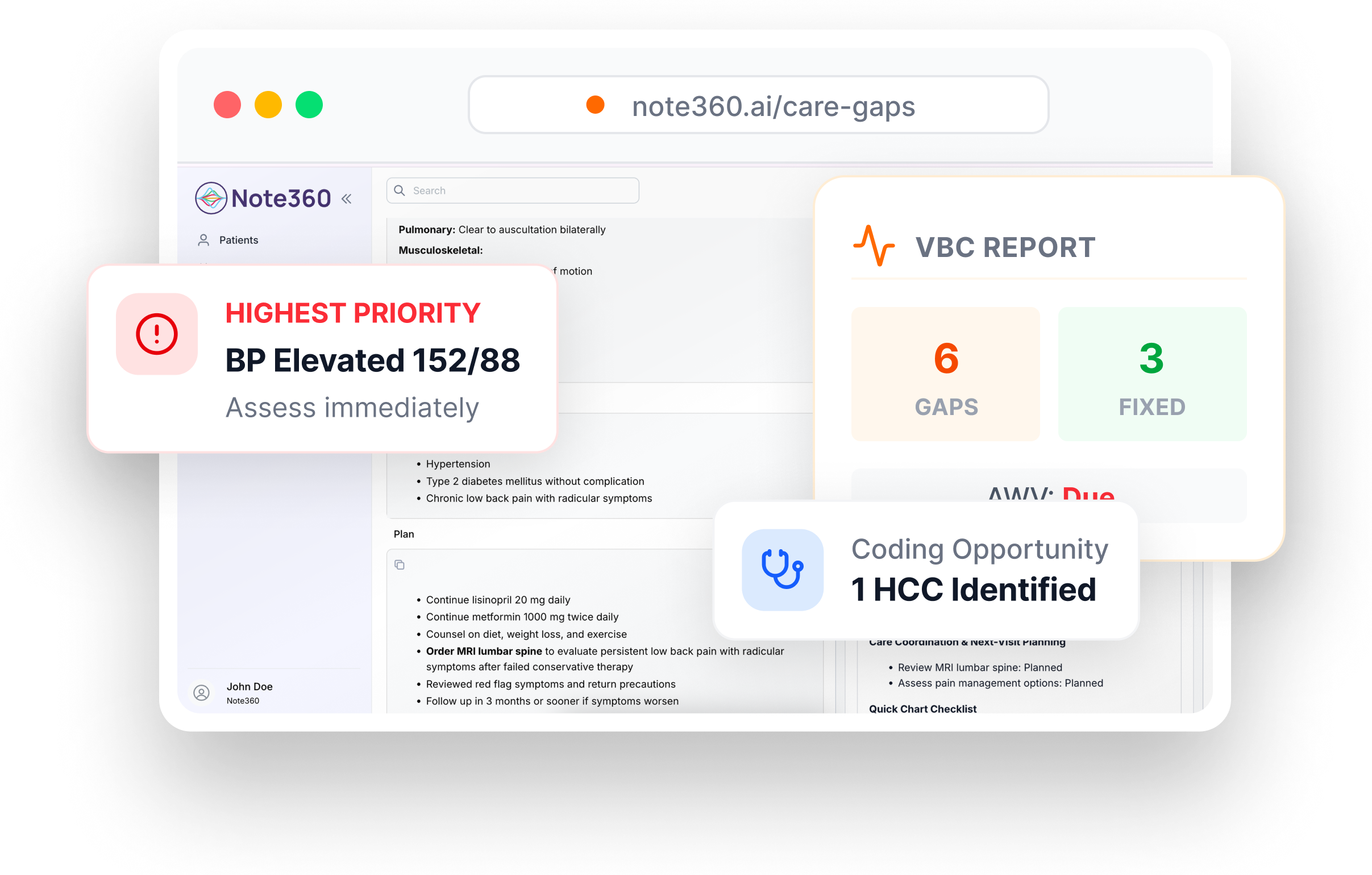
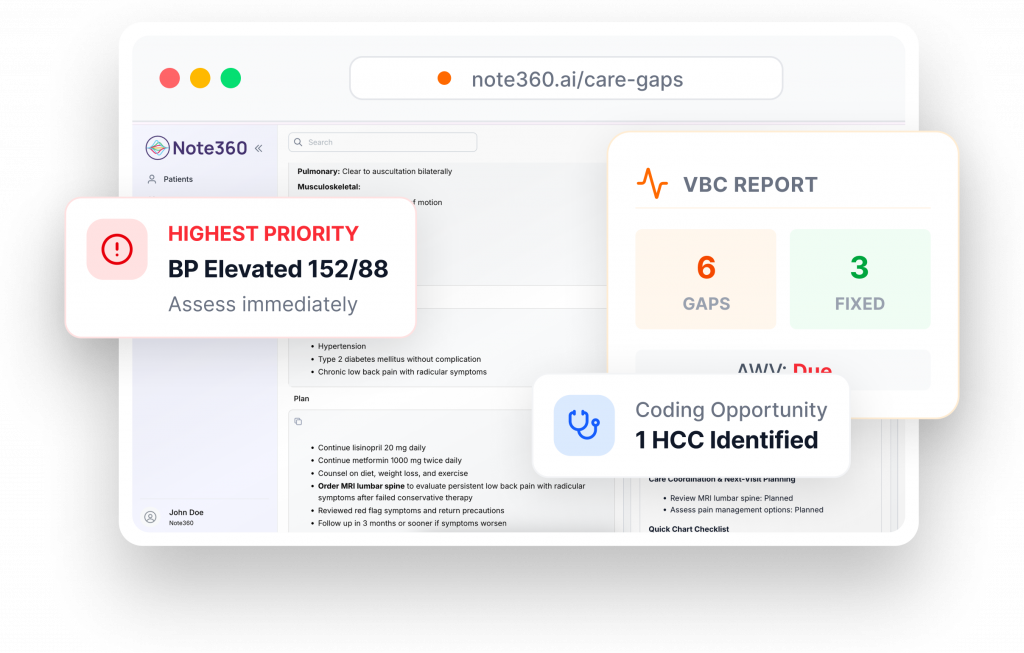
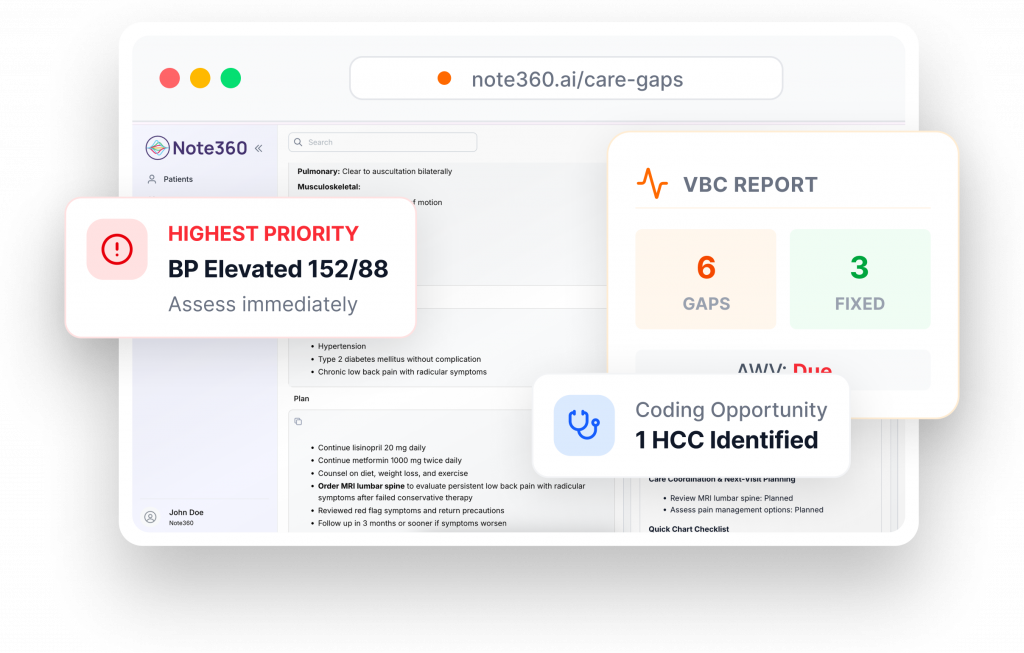
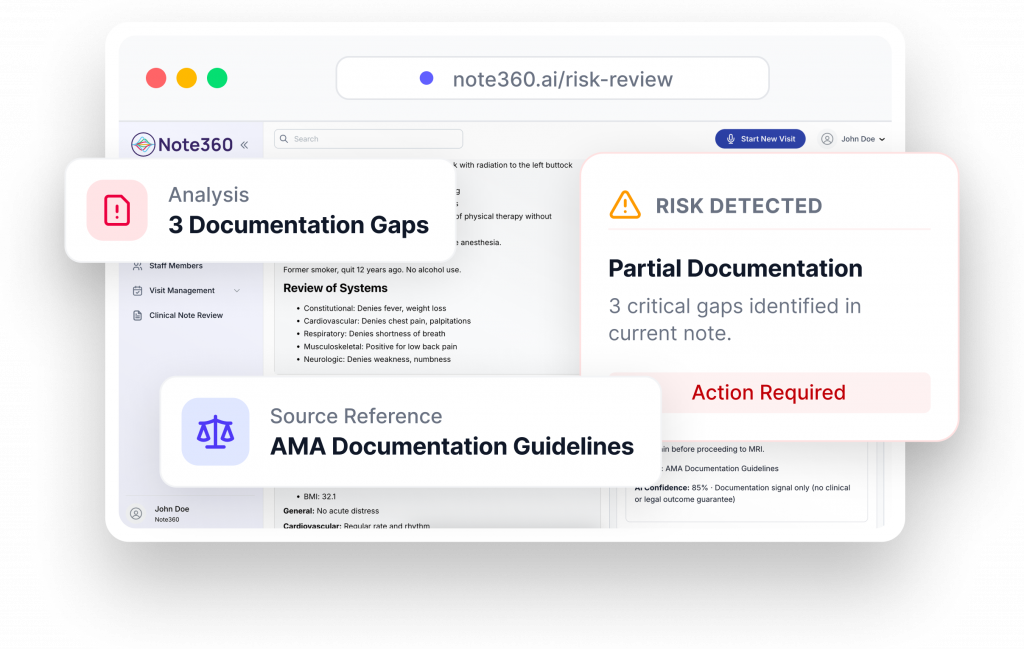
Identify documentation gaps that affect quality and continuity of care. Note360 brings visibility to missing or unclear documentation related to quality measures, risk adjustment, and longitudinal care. By surfacing these gaps earlier, teams can address them while context is still available.
How it helps
Surface documentation gaps before submission. Note360 provides real-time review and structured validation, so clinicians can focus on care, not corrections.